Chikungunya
Chikungunya is a mosquito-borne viral disease. The disease was first recognized in 1952 during an outbreak in southern Tanzania. It is a Ribonucleic Acid (RNA) virus that belongs to the alphavirus genus of the family Togaviridae. The name “chikungunya” derives from a word in the Kimakonde language of southern Tanzania, meaning “to become contorted”, and describes the stooped appearance of sufferers with joint pain (arthralgia).
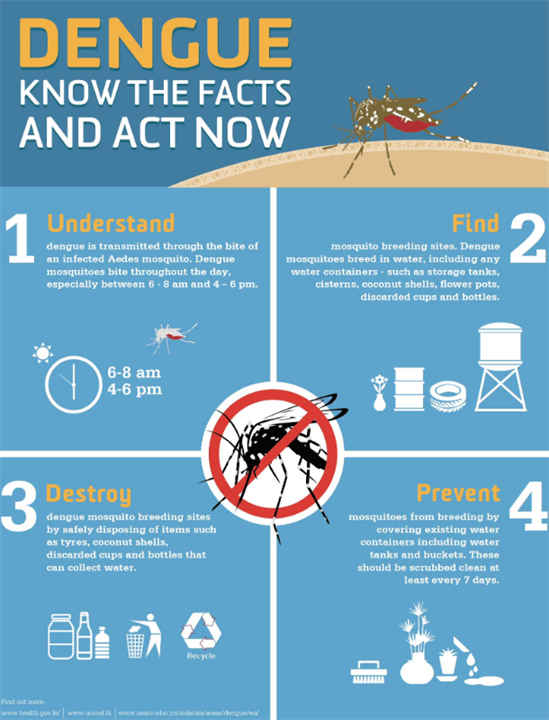
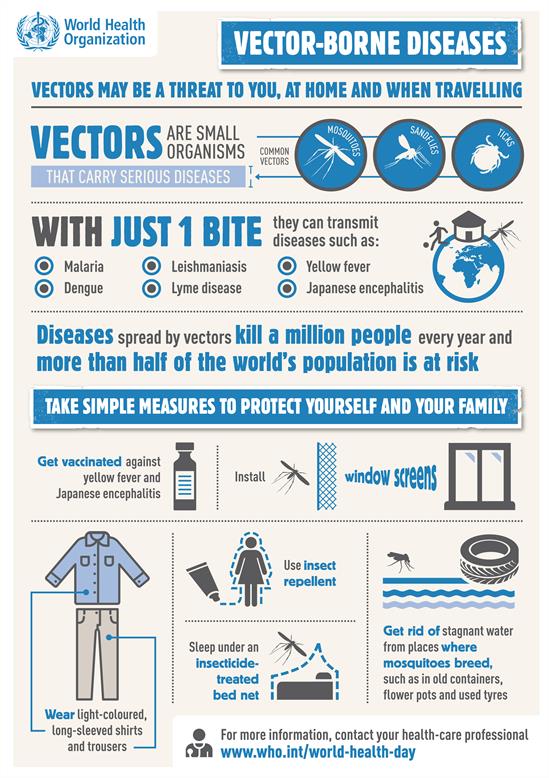
Chikungunya is transmitted to humans by the bites of infected female mosquitoes. Most commonly, the mosquitoes involved are Aedes aegypti and Aedes albopictus. These two species can also transmit other mosquito-borne viruses, including dengue. They bite throughout daylight hours, although there may be peaks of activity in the early morning and late afternoon.
Chikungunya is characterized by an abrupt onset of fever which is frequently accompanied by joint pain. Other common signs and symptoms include muscle pain, headache, nausea, fatigue and rash. The joint pain is often debilitating and usually lasts for a few days to a few weeks.
Most patients recover fully, but in some cases joint pain may persist for several months, or even years. Occasional cases of eye, nervous system and heart complications have been reported, as well as gastrointestinal complaints. Serious complications are not common, but in older people, the disease can contribute to the cause of death. Often symptoms in infected individuals are mild and the infection may go unrecognized or be misdiagnosed in areas where dengue also occurs.
Several methods can be used for diagnosis. Serological tests, such as enzyme-linked immunosorbent assays (ELISA), may confirm the presence of IgM and IgG anti-chikungunya antibodies. IgM antibody levels are highest 3 to 5 weeks after the onset of illness and persist for about 2 months. Samples collected during the first week after the onset of symptoms should be tested by both serological and virological methods (RT-PCR).
The virus may be isolated from the blood during the first few days of infection. Various reverse transcriptase–polymerase chain reaction (RT–PCR) methods are available but are of variable sensitivity. Some are suited to clinical diagnosis. RT–PCR products from clinical samples may also be used for genotyping of the virus, allowing comparisons with virus samples collected from patients in various geographical regions.
There is no specific antiviral drug treatment for chikungunya and there is no commercial chikungunya vaccine. Treatment is directed primarily at relieving the symptoms, including joint pain. This is largely achieved by using anti-pyretic drugs to reduce fever, by optimising the use of pain medication, and by administering fluids. Aspirin and other non-steroidal anti-inflammatory drugs should not be administered until dengue can be ruled out in order to reduce the risk of bleeding.
Prevention and control rely heavily on reducing the number of purposely-filled household containers (e.g., domestic water storage, decorative plants), as well as rain-filled habitats (e.g., used tyres, blocked gutters) that allow mosquitoes to breed. During outbreaks, insecticides may be: sprayed to kill flying mosquitoes; applied to surfaces in and around the abovementioned water-filled habitats where the mosquitoes land; and used to treat these habitats to kill the immature larvae.
For protection during outbreaks of chikungunya, clothing which minimizes skin exposure to day-biting mosquitoes is advised. Repellents can be applied to exposed skin or to clothing in strict accordance with product label instructions.
For those who sleep during the daytime, particularly young children or sick or older people, insecticide-treated mosquito nets afford good protection. Mosquito coils or other insecticide vaporizers may also reduce indoor biting.